Employers need to be aware that asthma is not just caused by dust, house mites or genetic inheritance, but the workplace can cause asthma and make symptoms worse for existing asthmatics.
Occupational factors account for about 1 in 6 cases of asthma in adults of working age with almost 90% of those cases being attributed to an allergic response to something in the workplace.
Occupational asthma has become the most common work-related lung disease in developed countries.
Different types of occupational asthma
Occupational Asthma- Sensitiser Induced Asthma
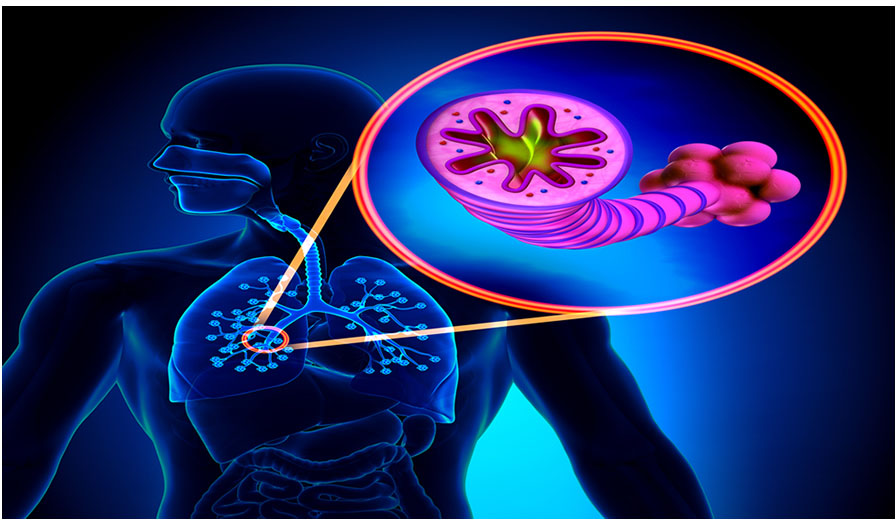
This is asthma that is caused as a direct result of workplace exposure to substances. These substances are called ‘respiratory sensitisers’ or asthmagens. They can cause a change in people’s airways, known as the ‘hypersensitive state’ meaning the airways to become extra sensitive to certain substances.
Your immune system’s job is to protect you from bacteria and viruses. If you are sensitised though, part of your immune system works too hard. It may attack harmless substances — like chemical fumes, or flour dust– in your nose, lungs, eyes, and under your skin.
When your body meets an allergen, it makes chemicals called IgE antibodies. They cause the release of chemicals like histamine, which cause swelling and inflammation. This creates familiar symptoms like a runny nose, itchy eyes, and sneezing as your body tries to remove the allergen.
If you have occupational asthma your immune system overreacts if the substances you are sensitised to enter the body. The muscles around your airways tighten. The airways become inflamed and over time are flooded with thick mucus causing difficulty breathing.
Not everyone who becomes sensitised goes on to get asthma and it can take months or years for the body to become sensitised to a substance; however once the lungs become hypersensitive, further exposure to the substance, even at quite low levels, may trigger an attack. Asthma can be life threatening and affect your ability to work.
Work related asthma- irritant induced asthma
This is when people with existing asthma is irritated or “triggered” by substances in the workplace. .e.g. when a worker breathes in an irritant substance like a chemical or dust. Symptoms tend to develop soon after the exposure (usually within 24 hours). Irritation can build up over time so it may take months of years of repeated exposure to trigger “work related asthma” symptoms.
Common symptoms to look out for:
The symptoms tend to be the same for both types of asthma so watch out for:
- Recurring soreness or watery eyes
- Recurring blocked or runny nose
- Chest tightness
- Wheezing
- Bouts of coughing
- Symptoms generally improving at weekends or during holidays
- The symptoms may develop immediately after exposure, or sometimes may appear several hours after exposure.
Industries most commonly affected
In the UK, workers that are affected most commonly from allergic occupational asthma are workers in food production, flour mills and bakeries, as well as those in car paint shops. This is due to the flour dust and amylase and isocyanates, the chemicals found in car paint sprays. A few examples of other workplaces vulnerable to occupational asthma are below:
- Woodworkers, employed in dusty environments.
- Solderers, affected by the fumes from rosin-based solder flux.
- Vets and other people working with animals may become sensitive to animal dander or dirty cage bedding.
- Workers exposed to car exhaust fumes.
- Health care workers exposed to latex or by products of diathermy (a surgical procedure).
- Metal workers (exposure to metal working fluids).
- Hairdressers exposed to chemicals like persulphate salts, henna, formaldeyde
The occupations with the highest incidence rates include bakers and vehicle paint sprayers. The most commonly cited cause of occupational asthma was isocyanates followed by flour. For a list of substances that have been identified as being ‘sensitisers’ go to www.hse.gov.uk/asthma/substances.htm
What can be done to help?
The best control measure is to eliminate or substitute the sentising agent for one that is not a known sensitiser. This is not always possible, so in this case you will need to control the exposure. This can be achieved at source for example by using engineering controls such as Local Exhaust Ventilation (LEV).
PPE is the last resort. Respiratory Protective Equipment (RPE) will reduce the incidence of the condition but not fully prevent it. To achieve optimum effect, it must be the correct type, fitted properly, well maintained and training should be provided for workers in wearing, removal, storage and replacement.
Preventing onset of the disease by eliminating or reducing exposure is the primary objective; a secondary method involves detecting early or pre-symptomatic disease. Where a risk of occupational asthma is identified health surveillance (usually consisting of a lung function test and symptom survey /respiratory health questionnaire before exposure e.g. on commencement of employment, and annually thereafter) should be provided. This can detect ill-health at an early stage and the outcome is improved in workers who are included in the programme.
If you have staff who are at risk of developing occupational asthma, get in touch with us today and we can help detect and respond to early signs and manage these. Contact us now to discuss any Health Surveillance requirements you may have.
If you would like to be added to our mailing list to receive informative articles similar to the above and other company updates, please click here.


